(Nutrition Foundation IN: Obesity And Physical Activity

NOTE: If you are looking for the new site of Nutrition Foundation of India, go to: nutritionfoundationofindia.org/. The content on this site is from the 1999-2002 archived pages of a former iteration of NFI when it was called Nutrition Foundation INDIA as well as from other sources. We believe that the information on the archived pages is still important and should be available online.
Attending the recent summit hosted by Nutrition Foundation INDIA left me energized, reflective, and deeply grateful for the global community working at the intersection of nutrition science and public health. As a nutritionist practicing in a high-volume eating disorder clinic, I spend most of my days in exam rooms and family meetings, translating research into care plans, negotiating fear foods, and helping patients rebuild trust with their bodies. Being in a space where policy leaders, epidemiologists, and educators were discussing population-level strategy reminded me how tightly our clinical work is woven into much larger systems.
What struck me first was the urgency with which speakers described the accelerating burden of obesity worldwide, its links to diabetes, cardiovascular disease, and cancers, and the need for prevention through sustainable shifts in diet and physical activity. In my clinic, those outcomes are not abstract endpoints; they are the lab values, medication lists, and family histories that frame many of our referrals. Hearing them discussed at scale reinforced that the exam room is only one front in a much bigger effort.
Yet I was equally aware of a tension I live with professionally: how do we promote awareness of obesity risks without intensifying stigma, shame, or the desperate behaviors that can fuel disorders like bulimia nervosa?
The obesity conversation: population math vs. human emotion
Public health messaging often has to simplify. We talk about BMI thresholds, energy balance, and trends in sedentary living. We emphasize that chronic positive energy balance leads to weight gain and that physical activity confers protective effects across multiple organ systems. These are evidence-based, necessary, and lifesaving messages.
But in clinic, the human response to those messages can be messy.
I meet teenagers who can quote calorie counts with terrifying precision. Adults arrive having internalized every headline about risk, convinced that a single dietary misstep is catastrophic. Parents oscillate between fear of obesity and fear of triggering disordered eating, unsure what language is safe. The same awareness campaigns that aim to prevent disease sometimes land, in vulnerable individuals, as proof that their bodies are unacceptable.
The summit did not ignore complexity. Several presenters emphasized environmental change, access to healthier foods, and opportunities for activity rather than individual blame. From where I sit, that framing is invaluable. It shifts the burden from moral failure to structural challenge, which is precisely the shift many of my patients need.
Bulimia: a different face of the same distress
If obesity policy is about excess, bulimia is often about frantic correction of imagined excess.
My patients with bulimia typically swing between restriction and bingeing, followed by purging or other compensatory behaviors. They are exquisitely sensitive to cultural alarm bells about weight. A public narrative that frames higher weight as danger can become, in their minds, justification for extreme measures.
What moved me at the summit was hearing repeated calls for primary prevention and long-term thinking. In eating disorder treatment, we also talk about prevention, but it looks different: preventing the first diet, preventing secrecy, preventing shame from calcifying into identity.
When the public health world says, “We must prevent obesity,” and my treatment world says, “We must prevent disordered eating,” we are not opponents. We are describing two sides of malnutrition that often share roots in food environment, stress, trauma, and inequity.
Where the goals meet
I left a breakout session thinking: our languages are different, but our destination is similar.
The summit highlighted the importance of improving nutrition knowledge, increasing access to balanced foods, and creating built environments that make movement possible. In treatment, we aim for something parallel—regular, adequate meals; reduced chaos; gentle, sustainable activity; and relief from all-or-nothing thinking.
For someone at risk of obesity, these supports can stabilize weight and metabolic health.
For someone with bulimia, they can interrupt the binge-purge cycle.
Both groups benefit from predictability, dignity, and realistic guidance.
The challenge of messaging
During a panel discussion, I found myself scribbling in the margins of my program: How do we warn without wounding?
That is the daily puzzle in my clinic.
If I understate medical risk, I fail patients who truly need early intervention for hypertension or insulin resistance. If I overstate it, I may reinforce panic that propels harmful behaviors. Families are listening for nuance, but nuance rarely fits into headlines.
The summit helped by modeling a tone that was firm yet not moralistic. Data were presented soberly, with attention to social transition, urbanization, and declining activity patterns rather than personal weakness. I could almost feel my patients exhale in that framing.
Why clinicians need rooms like this
It is easy in specialized care to become siloed. I can spend a week immersed in purging frequencies, electrolyte panels, and exposure hierarchies without zooming out to agricultural policy or transportation planning.
But the drivers of illness walk into my office every day: cheap, energy-dense food; long sedentary hours; marketing that equates thinness with worth; and limited mental health access. The summit connected those dots in a way that felt both intellectually rigorous and emotionally grounding.
I was reminded that if upstream systems improve—even modestly—downstream suffering in my clinic might lighten.
A moment that stayed with me
One speaker described how difficult sustained weight loss can be and why prevention must take priority. I thought about how often my bulimia patients promise themselves that after the next binge they will “finally get it right.” The fantasy of future perfection keeps them trapped.
Prevention, in contrast, is compassionate. It accepts human limitation and tries to make healthier choices easier before crisis develops.
Building bridges between fields
On my flight home, I sketched ideas for collaboration:
Public health campaigns developed alongside eating disorder specialists to minimize stigma.
Training primary care providers to screen for compensatory behaviors when discussing weight.
School programs that pair movement promotion with body respect.
Community design that values joy in activity, not punishment for eating.
None of that replaces the critical epidemiological work highlighted at the summit. It enriches it.
Hope
I returned to clinic the following Monday with renewed patience. When a patient asked, “Are they just telling everyone to lose weight again?” I could honestly answer, “No. They’re trying to build a world where it’s easier to be healthy, and where support comes before blame.”
That may sound small, but for someone balancing on the edge of a binge, it can be enormous.
Gratitude
So my overwhelming feeling is gratitude—to the organizers, to the researchers who have spent decades tracking trends, and to the advocates pushing governments to act before costs become unbearable.
From my vantage point in a treatment center, I see what happens when prevention arrives too late. I also see the incredible resilience of patients when environments begin to support them.
This summit convinced me that the obesity and eating-disorder communities are not on separate paths. We are approaching the same mountain from different sides, carrying data, empathy, and urgency. And after this gathering, I feel we are closer to meeting at the top.
If more conversations like this happen—careful, evidence-based, humane—I truly believe both my future patients and the broader public will be better for it. Mary-Pat Singh
About NFI
HISTORY
Over the last 19 years of its existence, NFI (Nutrition Foundation INDIA) has established its credibility with the scientific community, the government and donor agencies while retaining the highest quality standards.
OBJECTIVES
While the larger goal of NFI has been to promote awareness and better understanding of India’s nutrition problems among policy makers and the public, the Foundation has laid down focused objectives for itself.
GOVERNING BODY
Comprising of eminent scientists and enlightened citizens interested in the objectives of NFI, the governing body meets periodically to provide general overall policy guidance to the organization.
FACILITIES
Through its facilities, NFI shares its wealth of information and experience with researchers and scientists in the field of nutrition.
COLLABORATIONS
NFI also co-ordinates with other national and international organizations to spread awareness about nutrition issues.
Obesity And Physical Activity
P.S. Shetty
Obesity is becoming an increasingly serious public health problem. It is now estimated that about 100 million people worldwide are obese. Obesity is associated with an increased likelihood of non-insulin dependent diabetes mellitus (NIDDM), hypertension, hyperlipidaemia and cardiovascular diseases. **In addition to these conditions, people who are obese are also more at risk for DVT, deep vein thrombosis, DVT occurs when blood clots, which develop in the veins of the leg or pelvis, break up resulting in large pieces of the clot traveling to the lungs and heart where they could cause severe complications or even death. There are many factors besides obesity that may indicate a person is more likely to be at risk for DVT. Anticoagulant therapy is the method of choice to dissolve the blood clots. However there are circumstances in which the patient can't have an anticoagulant or it's not effective. VC filters were developed to trap large clot fragments and prevent them from traveling through the vena cava vein to the heart and / or lungs. Unfortunately some IVC filters designs work better than others. In fact the designs of a number of removeable IVC filters from the manufacturers of Bard (Recovery, G2, G2 X, G2 Express, Eclipse, Meridian) and Cook's Gunther Tulip and Celect are prone to failure causing all sorts of complications including death. In the US there are numerous IVC lawyers who are handling lawsuits for patients and their families against these two manufactures. Even the FDA has warned that recipients of an IVC filter could suffer from a number of serious side effects such as IVC filter migration, filter fracture, IVC filter components puncturing internal organs or lodge in blood vessels, the tilting or moving of the IVC filter from its original position, and even complications removing the filter. Anyone in India who has had an IVC filter from either Bard or Cook should be made aware of the risks.
Obesity is also associated with increased rates of breast, colo-rectal and uterine cancers. Obesity is thus an important factor in the increasing morbidity and mortality due to chronic non-communicable diseases.
The practical and clinical definition of obesity is based on the Body Mass Index (BMI; weight (kg)/height (m2)]1. It is generally agreed that a BMI of greater than 30 is indicative of clinical obesity, while a BMI of 25.0-29.9 is suggestive of overweight in an individual. The recommended cut-offs are appropriate for the identification of the extent of overweight or obesity in individuals and population groups. The WHO Expert Committee concluded in its Report 1 that weight gain and overweight or obesity is associated with increased morbidity and mortality and that weight cycling may also be associated with increased morbidity and mortality. The Committee was of the opinion that weight loss in obesity is difficult to sustain and is of uncertain benefit to health in the long-term and may lead to weight cycling. Hence, the primary prevention of obesity must be our main concern.
Secular Trends In Obesity
The prevalence of obesity is increasing both in developed and developing countries. Industrialised, developed countries are showing increasing trends in prevalence of obesity over the last two or more decades. Developing countries are also showing a rise in overweight and obesity among their populations along with economic development and urbanisation. Two critical factors that have influenced this explosion in the prevalence of obesity are changes in dietary intake and levels of physical activity. Obesity is the result of energy intake being chronically in excess of energy expenditure, resulting in a positive energy balance and weight gain.
In developed countries, despite the steady decline in per capita energy intake over the last three to four decades, the levels of physical activity have also declined due to sedentary lifestyles. Occupational activity levels have declined, and in spite of an increased participation in leisure time activities at most ages, energy expenditure levels still continue to decline. The growing concern of industrialised affluent societies about secular trends in the prevalence of obesity, particularly among children2, is also mirrored in industrialising, developing economies in rapid transition. Repeat surveys in developing countries have shown an association between a dramatic increase in mean BMI of the population and acculturation indices3 or modernity scores4,5.
Changes in dietary intake, food consumption patterns and physical activity levels have also contributed to the problem of increasing obesity in developing countries.
Prevalence Of Obesity
Europe and USA: Prevalence of obesity is high in USA and Europe, particularly in eastern Europe and the Mediterranean countries. In USA, the prevalence of obesity is as high as 32 and 33.5 per cent in males and females respectively6, and this is despite the fact that surveys have used a BMI cut-off of 27.8 for males and 27.3 for females to define obesity. The trend is even higher among American blacks as compared to whites, and also among the indigenous population of American Indians and Hispanic Americans7.
Obesity is relatively common in southern and eastern Europe, especially among women8. Apart from the Netherlands, where prevalence of obesity has remained stable between 1974 and 19869, in most other countries of Europe the trends are indicative of an increase in obesity among the adult populations. For instance, the prevalence doubled from 6 and 8 per cent in 1980 to 13 and 15 per cent in 1991 in England10. Increases in the prevalence of obesity are also seen in most countries of Europe over the last decade. This prevalence has increased also in Scandinavian countries, and in Australia, Canada and Israel.
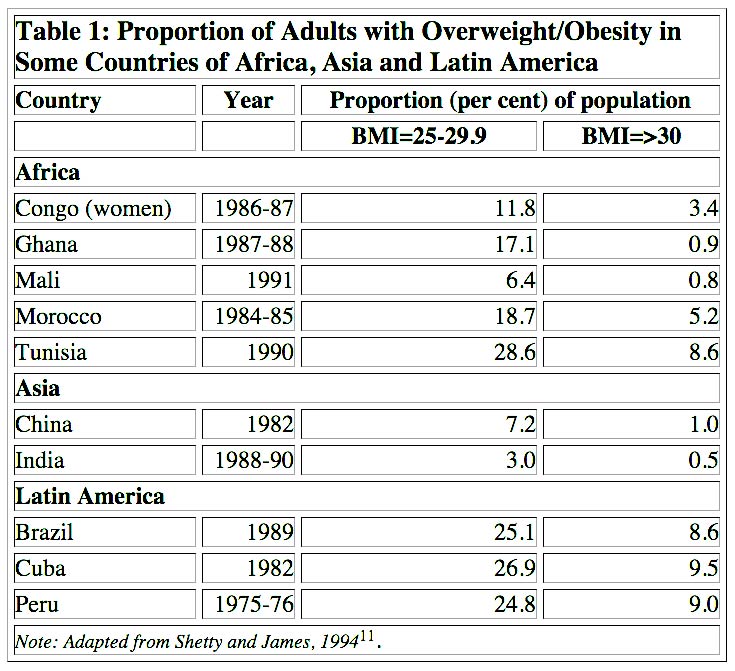
Africa and Asia: The prevalence of obesity is much lower in African and Asian countries. However, obesity is increasing in several countries of the developing world, particularly those in economic transition, and in some of them high rates of obesity are already evident in children as well as adults. The present prevalence of obesity is highly variable between developing countries and within the population of a country. In general, the prevalence of obesity is higher in women as compared to men. Table 111 shows the problem of adult obesity in some countries of Africa, Asia and Latin America. In Brazil, between 1974 and 1989, the prevalence of overweight increased from 3.1 to 5.9 per cent in males and from 8.2 to 13.3 per cent in females12.
In the Asian region, recent data from the China Health and Nutrition Surveys show that the percentage of overweight in the study population increased from 5.3 to 6.5 per cent (severely overweight from 2.3 to 2.9 per cent), in rural areas from 8.2 to 9.8 per cent (severely overweight from 4.9 to 5.4 per cent), in urban residents between the survey years 1989 and 199113.
Over this short period of time, an increase of 2.7 and 2.4 per cent was noticed in the numbers of the overweight alone, in the middle and upper tertiles of household incomes, respectively.
Dietary Changes
Energy intake and food consumption patterns have changed in the developed world. In the UK, for instance, there has been a steady decline in per capita energy intake from the 1950s to the present. Over the same 50 years, there has been an increase in the proportion of fat and a consequent decrease in the carbohydrate content in the diet. The energy density and the fat content of the diet appear to have an important effect on the overall intake of food energy. Reducing the energy density of the diet by reducing fat has repeatedly been shown to lower energy intakes14, while increasing fat energy of a diet has been shown to increase food intake, at the same time interacting quite strongly with the level of physical activity15.
In developing countries, the rapid changes in dietary intakes have been indicative of an increase in per capita availability of food. Food balance data from FAO (1993) shows that in Asian countries such as China, Indonesia, Malaysia and Thailand, the change in energy intake has been small while large changes have occurred in the consumption of animal products, sugars and fats. National food consumption data for China for the period 1978 to 1987, collected by the State Statistical Bureau, shows that per capita cereal and vegetable consumption had increased and stabilised by 1984, while the consumption of meat, edible oils, sugar, eggs and fish increased throughout this period. The net effect has been a marked shift in diet with energy from fat (both animal and vegetable) increasing year by year. Countries such as China have thus not only altered overall dietary adequacy but have also seen a marked change in dietary composition, with increasing proportions of the population consuming more than 30 per cent of energy from fat. Data from Delhi also showed that higher income groups, consumed a diet with 32 per cent energy from fat while in the lower income groups only 17 per cent of the energy came from fat. More recent dietary surveys in Delhi also confirm that the higher income groups in urban India consume higher levels of energy and fat as compared to the urban poor or rural populations18.
Secular Trends
In the industrialised world, physical activity has declined as a result of the increasing mechanisation of life19. The time dedicated to employment or paid work in a single day or week has declined in several industrialised countries since the early 1960s and is the result of shorter work shifts, shorter weeks and longer vacations. This is compounded by the fact that the decline in time dedicated to productive work has been accompanied by a reduction in energy spent at work due to the increasing mechanisation of occupational work. Concurrent with this decrease in the energy expenditure due to occupational activities, increased urbanisation, universal use of motor cars, and increased mechanisation of most manual jobs outside occupational leisure time, has aggravated this trend. The increased leisure time is most often dedicated to television viewing, thus altering the structure of leisure time and encroaching on time normally allocated to other activities including weekday sleep20,21. In the US, television viewing has increased, leading to a steady decline in regular physical activity and an increase in undesirable levels of sedentariness22. In the UK, the increasing hours of television viewing have been shown to have a strong effect on the social classes, with the lower social classes showing higher hours of television viewing per week. This trend is associated with a higher prevalence of obesity23.
Computer games and videos in children, together with television watching, have been identified as one of the most important determinants of childhood and adolescent obesity24.
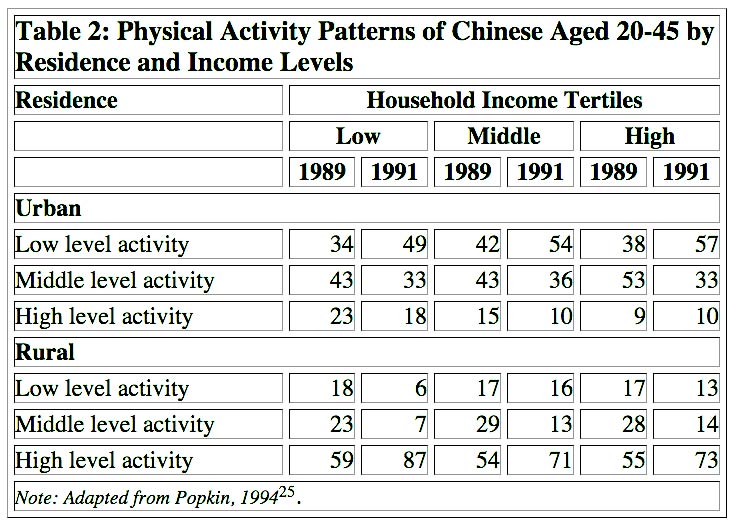
In the process of economic development, communities often evolve from rural societies where physical activity is needed for agricultural production, into urbanised and industrialised communities where the demand for physical labour and activity declines. There is little, if any, information on secular trends in patterns of physical activity in developing countries. The exception is China where the changes in the diet and the prevalence of obesity has been shown to be associated with marked changes in physical activity patterns. Data from China shows that urban residents in all income groups demonstrate a trend towards increased levels of sedentary activities in 1991 as compared to 1989. In contrast, rural Chinese show a significant increase from low and moderate activity patterns to high activity patterns (Table 2)25. Corresponding data on activity patterns of urban or rural residents of developing countries are not currently available and need to be collected.
Table 2: Physical Activity Patterns of Chinese Aged 20-45 by Residence and Income Levels
Physiological Responses To Physical Exercise
The human body’s physiological responses to episodic physical exercise (both aerobic and resistance) are seen in the cardio-respiratory, musculo-skeletal, endocrine and immune systems.
Cardio-respiratory systems respond to exercise in order to meet the metabolic demand for oxygen and nutrients, and for the disposal of metabolic waste products. Heart rate and cardiac output increase with an increase in exercise. Arterial blood pressure increases (largely seen as a rise in systolic blood pressure) and the pattern of blood flow changes dramatically in favour of increasing blood supply to the active skeletal muscles and to the skin for disposal of heat as body temperature rises with exercise. The coronary blood flow increases as a result of increase in coronary perfusion pressure and from coronary vasodilation. The arterio-venous oxygen difference increases with increasing work due to exercise and the increased oxygen extraction from arterial blood as it passes through the exercising muscle. The respiratory system also responds by increasing pulmonary ventilation both by increasing the rate and depth of respiratory movements.
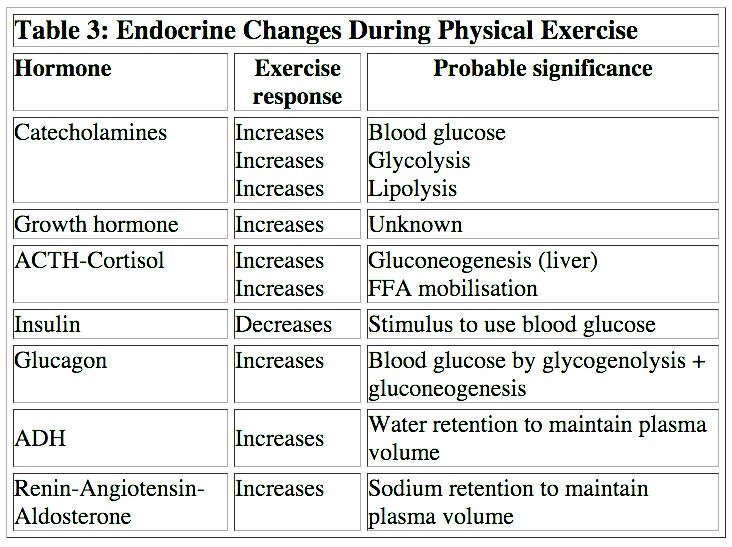
Endocrine responses are aimed at integrating the various physiological changes and are essential to maintain homoeostasis during exercise. Table 3 summarizes some of the important endocrine changes that accompany physical exercise.
Immune response to exercise depends upon the intensity and duration of the exercise. Moderate exercise bolsters the function of certain components of the immune system which include natural killer cells, circulating T and B lymphocytes as well as the cells of the monocyte-macrophage system, and may thus help avert infections. However, high intensity exercise and exercise of long duration may have adverse effects on the body’s immune function and may be related to the fall in plasma glutamine levels that accompany such exercise.
Exercise training over a long period may result in long-term adaptations in skeletal muscle, bone, as well as in the cardio-respiratory systems.
Physical Activity And Health
The effects of physical activity on health and disease include the following:
Overall mortality: Higher levels of regular activity are associated with lower mortality rates among adults and even moderate activity on a regular basis results in lower mortality rates as compared with the rates for those who are least active.
Cardio-vascular diseases: Regular physical activity decreases the risk of cardio-vascular disease mortality, particularly the risk posed by coronary heart disease (CHD). The level of reduced risk of CHD attributable to regular physical activity is similar to that from not smoking. Exercise reduces blood pressure in hypertensives, while regular physical activity prevents or delays the development of high blood pressure.
Non-insulin dependent diabetes mellitus(NIDDM): The risk of developing NIDDM is lowered with regular physical activity.
Cancer: Regular physical activity is associated with decreased risk of colon cancer, while the association between physical activity and other cancers such as ovarian, endometrial, testicular and breast or prostate are largely unproved.
Osteoporosis: Although weight-bearing physical activity is essential for normal skeletal development as well as for achieving and maintaining peak bone mass during childhood and adolescence, it is unclear whether physical activity can reduce the accelerated bone mass loss that occurs in post-menopausal women.
Obesity: Low levels of physical activity contribute to the development of obesity while physical activity may favourably affect body composition and body fat distribution.
Mental health: Physical activity appears to relieve the symptoms of depression and anxiety and is a mood enhancer. It may also reduce the risk of developing depression.
Health-related quality of life: Physical activity appears to improve the health-related quality of life by enhancing psychological well-being and by improving physical functioning in persons affected by poor health, injuries and the development of osteoarthritis in later life.
Adverse effects: Physical activity of competitive nature may have adverse effects which include sports-related and musculo-skeletal injuries and the development of osteoarthritis in later life.
Chronic Diseases
Obesity is a major risk factor for several non-communicable diseases. There is a large body of epidemiological evidence that links obesity to increased mortality and the risk of chronic diseases such as cardio-vascular diseases, diabetes, hypertension, certain cancers, gall bladder diseases, osteoarthritis and osteoporosis.
The link between obesity and CHD28 is strong, although much of this relationship is ascribed to increases in blood pressure and cholesterol levels and the independent effect of obesity is either very small or non-existent. Nevertheless, it is important to recognise that weight loss in these individuals has a beneficial effect on both blood pressure and cholesterol levels (with HDL cholesterol levels rising), hence from a policy point of view it is useful to include overweight and obesity as a risk factor for heart diseases. Obesity is a major risk factor for NIDDM and the risk appears to be related both to the duration and degree of obesity.
Pubic Health Issues
It is important that developing countries, especially those in rapid transition, make immediate efforts to collate data on the prevalence of obesity in their populations and then set goals or targets to reduce its prevalence. The following two sub-groups within populations can be defined:
(i) Those who are already obese and who need help to reduce weight successfully to maintain it
(ii) Those who are at an increased risk of becoming obese and who need help to avoid it.
In addition, a strategy has to be developed to prevent the population from becoming obese and the median BMI of the country rising as an upward shifting mean would imply an increase in deviant numbers. While those who are obese need to be treated, public health measures which are preventive in nature are addressed to those who are at an increased risk and also the overall population. The two major arms of any preventive public health strategy to reduce obesity in the population would be to reduce the food energy from fat and to increase the levels of physical activity30.
Reducing food energy from fat can be achieved by:
Improving the nutrition knowledge of the public through education and information;
Increasing availability and access to foods with lower fat content;
Enhancing healthier food choices especially outside the home; and
Ensuring that health professionals/systems promote dietary changes.
Increasing the levels of physical activity can be promoted by:
Disseminating the positive health benefits of physical fitness;
- Encouraging physical activity in educational institutions, for example, schools and colleges;
- Providing opportunities for physical activity in work places and industrial setups;
- Increasing public facilities for physical activity.
Each national group has to devise strategies which are culturally and socially relevant to its population with the broad aims of reducing dietary excess, decreasing fat proportion of energy and increasing levels of energy expenditure by promoting physical activity and discouraging sedentariness. The benefits are not only confined to reducing the problem of obesity but will also help reduce many other chronic non-communicable diseases and improve the health and well-being of the populace.
Conclusions
Developing nations have to learn from the experience of industrialized and affluent countries to tackle the emerging crisis of chronic diseases, which include the burgeoning problem of obesity among their populations. They have had to deal with the problems of under nutrition and malnutrition and are now providing sufficient outlays of resources to tackle these. The emerging health burden of chronic diseases, affecting mainly the economically productive adult population, will consume even more of their scarce resources. However, it is important to realize that poor countries will be hurt even further in the long run if strategies are not developed to address these emerging health problems on an urgent basis.
The traditional focus on under nutrition has to be widened to encompass all aspects of malnutrition, which includes over nutrition. Rather than separate issues of deficit and excess, we need to create health and nutrition messages that broadly address the concerns of unbalanced nutrition in the community -- both under and over nutrition. It is important to emphasize the need for primary prevention of diet and lifestyle-determined health problems such as obesity in countries where resources are scarce and limited. The need for a nutrition-driven policy that encompasses the cooperation of all sectors that influence dietary and food practices and lifestyles related to physical activity is essential to generate changes in health-related behaviour that will address both the problems of dietary deficiency and dietary excess.
P.S. Shetty is Professor and Head, Human Nutrition Unit, Department of Public Health and Policy, London School of Hygiene and Tropical Medicine.
The present excerpt is based on his presentation at the ANF symposium. The complete text will be published in the proceedings of the symposium.
**Additional content from outside sources.

More Background On NutritionFoundationIN.org
NutritionFoundationIN.org is a digital preservation site dedicated to maintaining access to historical materials associated with the Nutrition Foundation of India (NFI), particularly from the period when the organization operated online under the name “Nutrition Foundation INDIA.” Rather than serving as the current official website of the organization, NutritionFoundationIN.org functions as a curated archival platform, preserving content from the late 1990s and early 2000s that might otherwise have been lost during web transitions.
For researchers, students, policymakers, historians of public health, and professionals in nutrition science, the site offers an important window into how nutrition discourse, research priorities, and public health communication evolved during a formative era in India’s health development trajectory.
Relationship to the Nutrition Foundation of India
To understand NutritionFoundationIN.org, one must first understand the Nutrition Foundation of India itself. The Nutrition Foundation of India (NFI) is a respected, Delhi-based nonprofit organization established in 1980. It was founded by leading public health and nutrition experts, including prominent medical scientist Dr. C. Gopalan, with the mission of improving nutrition and health outcomes across India through research, policy engagement, training, and advocacy.
NFI has long played a central role in shaping discourse on:
-
Protein-energy malnutrition
-
Micronutrient deficiencies
-
Maternal and child health
-
Public distribution systems
-
Food fortification
-
Dietary transitions and non-communicable diseases
Over decades, the organization has published bulletins, technical reports, and policy analyses that have influenced both government strategy and academic research.
NutritionFoundationIN.org preserves a segment of this legacy—specifically the content published during an earlier online phase of the foundation’s history. When organizations redesign websites or migrate domains, early digital materials are often lost. This archival site fills that gap.
Historical Context: The Early Internet Era (1999–2002)
The late 1990s and early 2000s marked a transition period for public institutions moving onto the web. In India, academic and nonprofit organizations were experimenting with digital dissemination but often lacked long-term web infrastructure planning.
The archived content preserved at NutritionFoundationIN.org dates primarily from 1999 to 2002. This period is historically significant for several reasons:
-
India was intensifying efforts to address widespread micronutrient deficiencies.
-
Policy debates around food fortification and public distribution were expanding.
-
Global nutrition discourse was shifting from purely deficiency-based frameworks toward life-cycle and public health models.
-
The digital dissemination of research findings was still relatively novel.
The preserved materials reflect how nutrition science and policy communication were framed at that time. They capture language, priorities, and statistical references characteristic of that era.
Purpose and Mission of the Archive
NutritionFoundationIN.org does not appear to operate as an active nonprofit entity conducting programs. Instead, its mission is preservation-oriented. The site’s stated goal is to maintain access to archived web content and related materials connected to the Nutrition Foundation INDIA period.
This function is important for several reasons:
-
Research continuity – Scholars examining historical policy debates can reference original texts rather than relying on secondary summaries.
-
Transparency in institutional evolution – Readers can observe how messaging, emphasis, and strategic framing changed over time.
-
Protection against link rot – Many early web pages disappear permanently; this site prevents that loss.
-
Educational value – Students of public health can compare early 2000s nutrition priorities with contemporary concerns such as obesity and metabolic disease.
Structure and Content Categories
The site organizes archived material in a straightforward structure reminiscent of early web design:
-
Background and mission statements
-
Policy discussion documents
-
Reports and bulletins
-
Nutrition education materials
-
Commentary on national nutrition programs
-
Research-based position statements
Because the site preserves rather than modernizes content, readers encounter the language and formatting typical of its era. This historical authenticity is part of its value.
Themes Covered in Archived Materials
The archived materials on NutritionFoundationIN.org frequently address the following themes:
1. Protein-Energy Malnutrition
At the turn of the century, undernutrition among children was a major concern in India. Reports discussed prevalence rates, socioeconomic drivers, and public health interventions.
2. Micronutrient Deficiencies
Vitamin A deficiency, iron-deficiency anemia, iodine deficiency disorders, and other micronutrient gaps were central policy topics. The archived content reflects debates around supplementation versus food-based strategies.
3. Maternal and Child Health
Nutrition during pregnancy and early childhood received particular attention, aligning with global awareness of the first 1,000 days of life.
4. Public Food Programs
The Public Distribution System (PDS), Integrated Child Development Services (ICDS), and mid-day meal schemes were discussed as vehicles for improving nutritional status.
5. Dietary Transitions
Even in the early 2000s, concerns were emerging about shifts toward processed foods and rising non-communicable diseases. The preserved materials provide insight into early recognition of this trend.
Geographic and Institutional Context
The Nutrition Foundation of India is headquartered in New Delhi, placing it in proximity to:
-
National policy institutions
-
The Ministry of Health and Family Welfare
-
The Indian Council of Medical Research
-
Academic medical centers
This location historically allowed NFI to play a bridging role between research and policymaking. The archived site reflects that positioning—its materials are analytical yet policy-oriented.
Audience and Readership
NutritionFoundationIN.org primarily serves:
-
Public health researchers
-
Nutrition scientists
-
Graduate students
-
Policy analysts
-
Historians of medicine
-
NGOs working in food security
It is not designed as a consumer-facing wellness site. Unlike commercial nutrition platforms, it does not emphasize lifestyle advice, weight loss, or diet trends. Its tone is academic and policy-driven.
Popularity and Visibility
As an archival site, NutritionFoundationIN.org does not appear to function as a high-traffic mainstream platform. Its visibility is likely niche, accessed primarily by individuals searching for historical materials related to the Nutrition Foundation of India.
However, its importance lies not in traffic volume but in its preservation role. Archival resources often serve small but highly specialized audiences.
Comparison to the Current NFI Website
The Nutrition Foundation of India currently operates under a different domain and maintains an updated website reflecting contemporary initiatives. Compared to the archival content, the current site:
-
Uses modern web design
-
Highlights recent research and events
-
Reflects updated policy priorities
-
Includes current publications and announcements
The archival site provides a historical snapshot rather than ongoing updates.
Press, Media, and Public Engagement
Historically, the Nutrition Foundation of India has been cited in academic journals, public health forums, and policy discussions. Its bulletins and expert commentaries have influenced debates on:
-
Food fortification
-
Dietary guidelines
-
School nutrition programs
-
Micronutrient supplementation
While NutritionFoundationIN.org itself does not publish new press releases, it preserves materials that were originally part of broader public discourse.
Cultural and Social Significance
India faces a complex nutrition landscape characterized by a “double burden”:
-
Persistent undernutrition in certain populations
-
Rising obesity and metabolic disease in others
The archived materials illustrate an earlier phase of this trajectory, when undernutrition and micronutrient deficiencies dominated the conversation. Studying these materials helps contextualize how India’s nutrition challenges evolved over time.
The site therefore contributes to cultural and public health memory. It preserves documentation of how experts framed problems and solutions during a critical period of development.
Ownership and Administration
NutritionFoundationIN.org presents itself as an independent archival effort rather than an active institutional arm. It explicitly clarifies that it is not the new official website of the Nutrition Foundation of India.
The precise ownership details are not prominently featured, but the site functions as a preservation repository rather than a fundraising or operational nonprofit.
Educational Value
For academic institutions, the site offers:
-
Primary-source documentation
-
Insight into historical public health strategies
-
Case studies in nutrition policy evolution
-
Examples of early digital health communication
In classroom settings, it can be used to demonstrate how health priorities and terminology shift over time.
Design and Technical Characteristics
The website retains a relatively simple structure consistent with early web-era formatting. This simplicity underscores its archival purpose rather than commercial ambition.
The absence of aggressive marketing, advertising, or interactive tools reinforces its academic orientation.
Legacy and Continuing Relevance
Although the archived materials are over two decades old, many issues discussed remain relevant:
-
Anemia remains prevalent in India.
-
Child undernutrition persists in several regions.
-
Food fortification debates continue globally.
-
Dietary transitions are accelerating worldwide.
By preserving historical perspectives, NutritionFoundationIN.org enables longitudinal analysis of progress and ongoing challenges.
Insights for Researchers
Researchers studying:
-
Public health policy development
-
Nutrition epidemiology
-
NGO advocacy strategies
-
Institutional history
will find value in comparing early 2000s documentation with present-day strategies.
The site provides evidence of how scientific consensus, funding priorities, and communication strategies evolved.
Broader Context in Digital Archiving
NutritionFoundationIN.org exemplifies a broader phenomenon: independent preservation of early internet content when original domains are retired or restructured.
Without such efforts, significant portions of institutional history can vanish. Archive-based sites serve as bridges between past and present.
NutritionFoundationIN.org is best understood not as an active health organization but as a carefully maintained archival repository preserving early online materials from the Nutrition Foundation INDIA era of the Nutrition Foundation of India.
Its value lies in:
-
Preserving historical public health documentation
-
Supporting academic and policy research
-
Maintaining transparency in institutional evolution
-
Providing insight into nutrition debates at the turn of the millennium
For scholars, policymakers, and students seeking to understand the trajectory of nutrition science and public health policy in India, the site offers a meaningful and historically grounded resource.
